At ADInstruments, we’re lucky to be part of an ever-growing community of scientific innovators.
These teams and individuals are constantly pushing the limits, developing new techniques and practices to run their experiments. We’re witnessing a new wave of cutting-edge research using our fully implantable Kaha telemeters.
Below we highlight just a few high-impact articles from researchers using Kaha telemeters.
Kaha Sciences Telemetry – High-Impact Research:
Understanding the relevance of pre-stroke hypertension
An ischemic stroke occurs when the blood supply to an area of the brain is interrupted, reduced, or completely cut off. This loss of blood supply results in a cascade of cell death. As brain cells run out of oxygen and nutrients, they die, rupture, and trigger cell death in surrounding cells.
In their initial investigation, covered in our first High-Impact Telemetry Blog, Thakkar et al. examined the impact of acute transient hypertension which occurs in 80% of patients after an ischemic stroke.

It had been suggested that, while dangerous, hypertension could be a protective mechanism to combat the increase in intracranial pressure poststroke. Thakkar et al. determined that post-stroke hypertension served no protective purpose, and blood pressure levels should be treated to return to normotensive/pre-stroke levels.
This follow-up investigation explores whether those results can be generalized to rats that had been hypertensive prior to their ischemic stroke.
The majority of stroke patients, around 60%, have a known background of hypertension. Roughly half of all stroke patients are on antihypertensive medications at the time of their stroke, and a further 15% are believed to have undiagnosed hypertension. Due to the critical nature of ischemic events, it can be difficult to determine whether a patient’s blood pressure during a stroke is the same as their normal daily blood pressure. However, given that we know that many patients will have been living with high baseline blood pressure, there may be a danger in bringing their blood pressure down to non-hypertensive levels after stroke.
Animals were divided into six experimental groups, however, in this overview, we will only discuss the following:
- Uncontrolled - no blood pressure interventions given
- Controlled - poststroke blood pressure treated to pre-stroke baseline
- Overcontrolled - poststroke blood pressure treated to normotensive levels
- Sham - sham stroke and vehicle injections
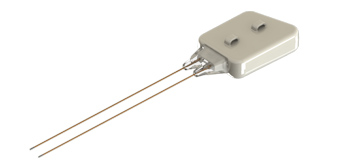
For thirteen days - three before and ten after an induced ischemic stroke - blood pressure and intracranial pressure were measured using an implanted Kaha Dual Pressure Telemeter, and brain tissue oxygenation was measured using an implanted Kaha Tissue Oxygen Telemeter.
As expected from Thakkar et al.’s previous study, preventing blood pressure from increasing after a stroke had no negative impact. However, reducing blood pressure below the pre-stroke baseline resulted in several significantly harmful effects. Intracranial pressure increased, putting excess strain on already damaged tissue. Cerebral perfusion pressure was reduced, allowing the area of damage to spread further as tissue received less oxygen and nutrients. Mortality increased. Infarct volume increased. Finally, Thakkar et al. noted that functional recovery progressed more slowly.
With such a high proportion of ischemic stroke patients believed to be living with hypertension prior to their ischemic event, these results demonstrate a need to review the existing guidelines for treating poststroke hypertension in order to avoid causing more harm.
Telemeters Used
Publication:
Thakkar, Pratik C., et al. “Therapeutic Relevance of Elevated Blood Pressure After Ischemic Stroke in the Hypertensive Rats.” Hypertension, vol. 75, no. 3, 2020, pp. 740–47. Crossref, https://doi.org/10.1161/hypertensionaha.119.14219.
Related: Getting started with small animal Telemetry: Fiona’s top three tips »
Heart rate variability is dissimilar to vagal tone
The vagus nerve is the largest nerve in the autonomic nervous system, innervating the heart, lungs, and digestive system. The signals it carries from the brain to the body are automatic, and part of the many non-conscious activities the body carries out in order to function.
It is nearly impossible to record from the vagus nerve in an accurate and safe manner in non-anesthetized animals, and not much more manageable in unconscious animals.

To circumvent this, heart rate variability (HRV) is often used as an equivalent measure. This is based on the assumption that HRV is driven primarily by vagus nerve activity and is therefore an appropriate measure of ‘vagal tone’. Abnormal ‘vagal tone’ has been associated with poor patient outcomes, and an increasing number of diseases from epilepsy to heart disease, diabetes, and depression. Vagus nerve stimulators are currently in development to treat these diseases.
This paper by Marmerstein et al. had two aims. Firstly, to examine the relationship between vagus nerve activity and HRV, aiming to test the long-held belief that HRV and vagal tone are equivalent. Secondly, to determine if the vagus nerve is an appropriate target for stimulator treatments.
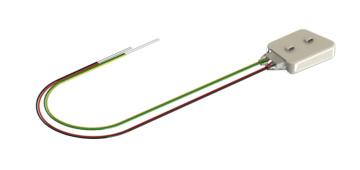
Recordings from freely moving and anesthetized rats were collected over 11 weeks using a combination of custom ultra-low noise electronics, ensuring the most accurate and generalizable data. Heart rate variability was recorded using an implanted Kaha Dual Biopotential Telemeter, while vagus nerve activity was recorded using carbon nanotube yarn electrodes developed by Marmerstein et al.
There isn’t a consensus regarding the kind of heart rate variability most closely related to ‘vagal tone’. To cover all their bases, Mamerstein et al. assessed the six most common measures in both time and frequency HRV domains:
- The standard deviation of the R-R interval
- The standard deviation of heart rate
- Root mean square of successive differences
- High-frequency power
- High-frequency power as a percentage of total power
- Low-frequency to high-frequency power ratio
Data was collected for 11 weeks. There was no significant correlation between HRV and vagus nerve activity in either anesthetized or awake, free-moving animals. This suggests that HRV is not a valid stand-in for ‘vagal tone’ with or without anesthetic.
The article goes on to examine respiration as a more accurate measure of ‘vagal tone’, and is well worth reading to see the details of the high correlation between vagus nerve activity, inspiration, and expiration.
Telemeter Used:
Kaha Dual Biopotential Telemeter (ECG, EEG and/or EMG) »
Publication:
Marmerstein, Joseph T., et al. “Direct Measurement of Vagal Tone in Rats Does Not Show Correlation to HRV.” Scientific Reports, vol. 11, no. 1, 2021. Crossref, https://doi.org/10.1038/s41598-020-79808-8.
Estrogen inhibition of salt-dependent hypertension
Hypertension, sustained high blood pressure, is a risk factor for a broad range of diseases; from stroke to heart disease to renal dysfunction. Surprisingly, one of the most protective factors against developing hypertension is being female. Before menopause, women are much less likely to develop hypertension than age-matched men, and it is less severe if they do develop hypertension.
This effect appears to be related to estrogen. Post-menopausal women, and those who’ve had their ovaries removed, no longer have this protective effect.
However, the protection reappears when these women are given estrogen replacement therapy.
In this Cardiovascular Research article, Jin et al. sought to determine the mechanism by which estrogen is able to block, or minimize, the development of hypertension. The team split the rats into two primary groups, with four and three further subgroups respectively:
Induced Hypertension
- Female - Sham ovariectomy
- Female - Ovariectomy
- Female - Ovariectomy and estrogen replacement
- Male
No Induced Hypertension
- Female - Sham ovariectomy
- Female - Ovariectomy
- Female - Ovariectomy and estrogen replacement
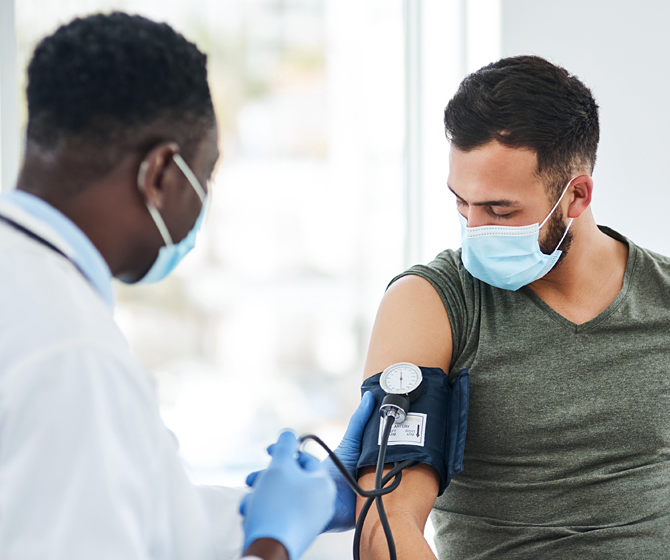
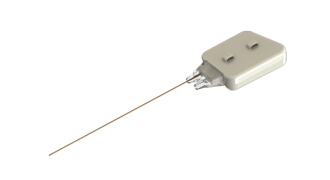
Hypertension was induced by removing one kidney from each rat, and supplying them with a 1% NaCl solution as drinking water for the 40-day experimental period. Blood pressure was measured using three methods: a tail cuff, directly through a polyethylene catheter, and chronically via an implanted Kaha Pressure Telemeter.
As expected, male and female rats that had their ovaries removed, and received no estrogen replacement, developed hypertension at roughly the same rate over the course of the experimental period. Meanwhile, the other rats in the ‘Induced Hypertension’ groups maintained blood pressure more in line with the ‘No Induced Hypertension’ animals.
Jin et al. hypothesized that estrogen inhibited the release of arginine-vasopressin (AVP), a hormone released in response to chronic salt intake. Animals in the above groups were given an IV transfusion of either 10, 100, or 1000 ng/kg bodyweight AVP. The effects were consistent across all groups with a dose-dependent blood pressure increase no matter the estrogen levels of the rats. This suggested that estrogen was protective against the release of AVP but ineffective at counteracting AVP once it was in the blood.
The team went on to examine estrogen effects on the GABAergic excitation of AVP neurons, AVP receptor modulation, whether a similar mechanism exists in male rats, and a potential pharmaceutical treatment targeting this system. See their Cardiovascular Research paper for more on these findings!
Telemeter Used:
Kaha Pressure Telemeter »
Publication:
Jin, Xiangyan, et al. “Oestrogen Inhibits Salt-Dependent Hypertension by Suppressing GABAergic Excitation in Magnocellular AVP Neurons.” Cardiovascular Research, vol. 117, no. 10, 2020, pp. 2263–74. Crossref, https://doi.org/10.1093/cvr/cvaa271.
Related: Five Unique Neuroscience Applications Using Telemetry »
For more information about Kaha Sciences telemeters, or to discuss your specific research application, please contact your nearest ADInstruments support representative.
Related resources:
Four benefits of telemetry for research »
Kaha Telemeters Cardiovascular Applications »
Exploring ICP, Tissue Oxygenation and RSNA with Implantable Telemetry »
How to measure chronic intracranial pressure measurements in rats »