At ADInstruments, we’re lucky to be part of an ever-growing community of scientific innovators.
These teams and individuals are constantly pushing the limits, developing new techniques and practices to run their experiments. We’re witnessing a new wave of cutting-edge research using our fully implantable Kaha telemeters.
Below we highlight just a few high-impact articles from researchers using Kaha telemeters.
Kaha Sciences Telemetry – High-Impact Research:
The Neuroprosthetic Baroreflex
This article from Nature covers the broad expanse of work completed to develop the neuroprosthetic baroreflex; an epidural stimulator that stabilizes hemodynamics after spinal cord injury. Hemodynamic stability, the regulation of blood pressure, is one of many automatic processes that can be diminished or eliminated by spinal cord injury. Without it, regulating blood pressure becomes more difficult, and something as minor as sitting up can cause loss of consciousness. This interferes with rehabilitation while also increasing the risk of stroke and heart disease.
Squair et al. began their investigation by characterizing a pre-clinical model of hemodynamic instability in TH-Cre rats. Using AAV infusions, they labeled neurons downstream of the rostral ventrolateral medulla (RVLM) - the region responsible for homeostatic control of sympathetic cardiovascular function. When given a clinically-relevant contusion to the upper thoracic spinal cord (T3) the model revealed that this neurological control of the cardiovascular system ended at the point of injury.
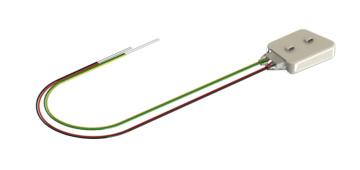
The impact of the injury on sympathetic cardiovascular control was characterized by long-term use of
Kaha SNA and Pressure Telemeters measuring sympathetic renal nerve activity and arterial blood pressure. The data from long-term implantable telemeters allowed the team to better understand how the hemodynamic instability changed as the rats recovered, as well as the types of activities that could work as reliable hemodynamic challenges for future testing.
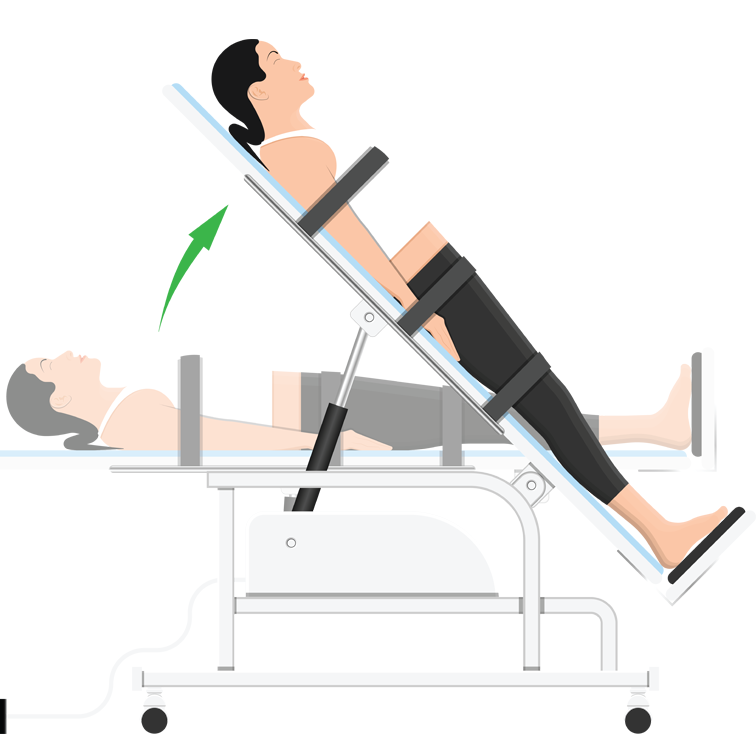
For humans, laying on a table that is then tilted up or down (a tilt-test) is the most common hemodynamic challenge. By examining long-term telemetry data, Squair et al. determined that this method wouldn’t be effective when testing rats. Instead, they created a negative pressure chamber which covered the rat from mid-abdomen downward, pulling blood toward the hindlimbs. Uninjured rats could quickly adapt to this pressure change, maintaining their blood pressure. Injured rats not only could not maintain their blood pressure but struggled to return it to normal even after the negative pressure eased; the same as a human with a spinal cord injury during a tilt-test.
This is just the start of the meticulous work carried out by Squair et al., which goes on to cover:
- The identification of spinal cord segments that restore hemodynamic stability when stimulated.
- The creation of an epidural stimulator for the rat model.
- Use of machine learning to provide naturalistic stimulation to these spinal cord segments, completely restoring hemodynamic stability.
- Translation of these tools and methods to a non-human primate, completely restoring hemodynamic stability.
- Pre-clinical translation into a human volunteer; again, completely restoring hemodynamic stability.
Telemeter Used:
Kaha SNA and Pressure Telemeter »
Publication:
Squair, Jordan W., et al. “Neuroprosthetic Baroreflex Controls Haemodynamics after Spinal Cord Injury.” Nature, vol. 590, no. 7845, 2021, pp. 308–14. Crossref, https://doi.org/10.1038/s41586-020-03180-w.
Related: Webinar: Next-Generation Techniques for Understanding Neural Hemodynamic Control »
Hypertensive Response to Ischemic Stroke
An ischemic stroke occurs when blood supply to an area of the brain is interrupted, reduced, or completely cut off. This loss of blood supply results in a cascade of cell death as brain cells run out of oxygen and nutrients, die, rupture, and trigger cell death in surrounding cells. During initial treatment, every second counts, but even after the blood supply is returned the danger isn’t over.
More than 80% of ischemic stroke patients develop acutely high blood pressure in the hours and days after their stroke. This increased blood pressure can be deadly, causing further strokes, heart attacks, aneurysms, and cerebral edema.
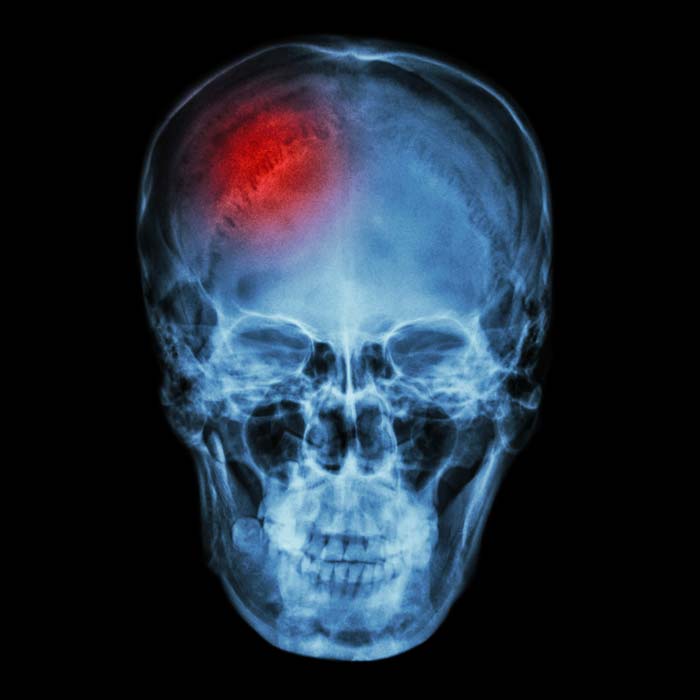
Clinical guidelines recommend controlling post-stroke hypertension with anti-hypertensive medications. It was unclear, however, whether reducing blood pressure could itself be harmful.
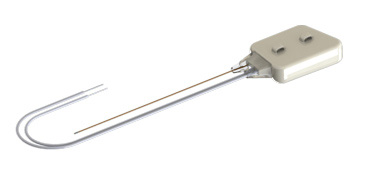
Thakkar et al. first explored the impact of controlling post-stroke hypertension in rats that had normal blood pressure before their ischemic stroke. There was a chance that, due to the increased intracranial pressure created by the stroke, the increased blood pressure may have been protective; forcing blood to keep moving in a higher pressure environment. Blood pressure and intracranial pressure were measured using an implanted Kaha Dual Pressure Telemeter, and brain tissue oxygenation was measured using an implanted Kaha Tissue Oxygen Telemeter
In all groups, blood pressure returned to normal levels around 4 days after stroke. By day 3, there was no difference in blood pressure between the treated and untreated rats. The most impactful result, however, was the lack of difference in brain tissue oxygenation between treated and untreated rats. Increased blood pressure offered no benefits to post-stroke rats, not for the health of damaged neural tissue nor in the recovery of sensorimotor function.
One reason for this may be that post-stroke hypertension also increases intracranial pressure. While some increase in intracranial pressure was found in both treated and untreated animals, the increase for treated animals was significantly smaller. Not only was post-stroke hypertension not protective, but it exacerbated the very issue it had been hypothesized to protect against.
Telemeters Used:
Kaha Dual Pressure Telemeter »
Kaha Tissue Oxygen Telemeter »

Publications:
Thakkar, Pratik, et al. “Hypertensive Response to Ischemic Stroke in the Normotensive Wistar Rat.” Stroke, vol. 50, no. 9, Ovid Technologies (Wolters Kluwer Health), Sept. 2019, pp. 2522–30. https://doi.org/10.1161/strokeaha.119.026459
Related: Getting started with small animal Telemetry: Fiona’s top three tips »
Cardiac Effects of Repeated Focal Seizures
Sudden Unexpected Death in Epilepsy (SUDEP) is an unpredictable killer. With no known mechanism of action it is unclear why and how it happens, and who might be at risk. What we do know is that generalized tonic-clonic seizures, and heart arrhythmia during seizures, are associated with SUDEP. It is likely that heart and respiratory problems are the cause of SUDEP and that repeated seizures may lead to fatal arrhythmias.
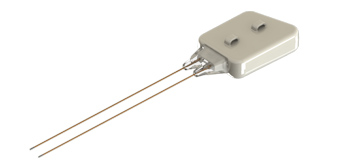
Jeffreys et al. explored the cardiac impact of recurrent seizures in a rat model, developing a clearer pathophysiology of these potentially fatal arrhythmias. Five animals were monitored for seven full weeks using implanted Kaha Dual Biopotential Telemeters, providing constant electrocardiogram (ECG) and cortical electroencephalogram (ECoG) data. After recording 6-14 days of baseline data, the rats received intrahippocampal injections of tetanus neurotoxin (TeNT), a treatment known to cause spontaneous epilepsy from an area of the brain unrelated to cardiac function.

This ensured that the treatment itself, and the resulting seizures, were not directly impacting the cardiac function of the animal; therefore, all cardiac changes were due to the wider physiological impact of the seizures.
The seizures began a few days after the TeNT injection. Treated animals would have groups of seizures, around 10 to 40 over a few days, with a day or so of no seizures between each group. During a seizure it was common for the telemeters to record tachycardic readings. The significantly increased heart rate could continue for more than 10 minutes after the seizure was over. As the experiment went on, the rats’ resting heart rates increased, showing lasting stress on their hearts outside of each seizure event. The severity of this effect was related to the severity of the seizure. If the rat had a Racine Class 5 seizure, a full motor seizure, the impact of their cardiac function was significantly worse than if they’d had a more mild seizure.
These arrhythmias, however, did begin to reverse. After week 3, seizures became less frequent and less intense. As this recovery period extended, the rat cardiac readings started to move back toward their baselines. It was the intense clustering of severe seizures reinforcing cardiac arrhythmia, and without that reinforcement the body began to return to normal. The less rest between seizures, the greater the intensity of those seizures, the worse the arrythmias became. This clear pathophysiology of epilepsy-induced arrhythmia gives us a much better understanding of who is at risk, and how that risk increases or decreases over the course of the illness.
Telemeter Used:
Kaha Dual Biopotential Telemeter (ECG, EEG and/or EMG) »
Publication:
Jefferys, John G. R., et al. “Cardiac Effects of Repeated Focal Seizures in Rats Induced by Intrahippocampal Tetanus Toxin: Bradyarrhythmias, Tachycardias, and Prolonged Interictal QT Interval.” Epilepsia, vol. 61, no. 4, 2020, pp. 798–809. Crossref, https://doi.org/10.1111/epi.16479
Related: Five Unique Neuroscience Applications Using Telemetry »
For more information about Kaha Sciences telemeters, or to discuss your specific research application please contact your nearest ADInstruments support representative.
Related resources:
Four benefits of telemetry for research »
Kaha Telemeters Cardiovascular Applications »
Exploring ICP, Tissue Oxygenation and RSNA with Implantable Telemetry »
How to measure chronic intracranial pressure measurements in rats »

