Ever wondered what the difference is between a Langendorff and a Working Heart perfusion model? Well, you’re probably not the only one!
While both are used for isolated heart studies - investigating the physiology and pharmacology of the heart without interference from the rest of the body, fundamentally they are different. These differences arise in the way that the heart is perfused, and will ultimately allow you to measure different cardiovascular parameters.
So how do you know which is the best solution for you? To help out, we have created a short guide outlining the main differences between Working Heart and Langendorff perfusion models. Enjoy!
Working Heart Perfusion
In a Working Heart model, the flow of the perfusate is designed to mimic the flow of the blood in situ. The perfusate enters the left atrium via the pulmonary vein, where it is pumped to the left ventricle and out through the aorta against a resistance, designed to replicate the systemic vascular resistance of the body.
As the name implies, this set up allows the heart to perform its physiological pumping action, so the user can simultaneously monitor mechanical and electrical cardiac parameters, to examine the influence of preload and afterload on cardiac work during perfusion. This set up is particularly useful for studying cardiac metabolism, pharmacological interventions, and loading conditions.
Working heart system parameters include:
- Aortic Pressure (Afterload)
- Left Atrial Pressure (Preload)
- Aortic Line Systolic & Diastolic
- Biphasic Action Potentials “ECG”
- Heart Rate
- Temperature

See here for more information about our working heart systems.
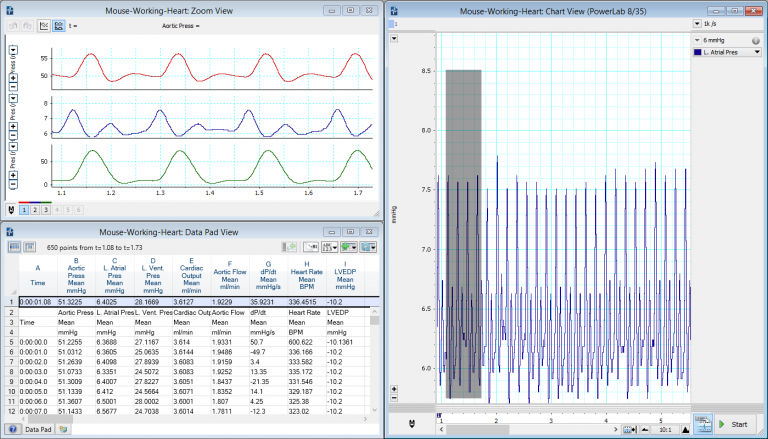
A typical Working Heart recording in LabChart (mouse model) featuring aortic, atrial and LV pressures, flow, and dp/dt.
Langendorff Perfusion
Unlike the working heart model, the Langendorff system relies on retrograde perfusion of the heart (through the coronary vasculature) in order to maintain cardiac function. This means the perfusate does not enter the left ventricle.
In brief, the technique involves cannulation of the aorta, which upon perfusion results in the closing of the aortic valve, thereby preventing flow into the left ventricle. Instead, the perfusate passes from the aortic root via the ostia, into the coronary vasculature providing the nutrients and oxygen required to maintain the physiological function of the heart.
By inserting a balloon into the left ventricle and connecting it to a pressure transducer, LV pressures can be measured during diastole and systole.
This set up allows you to record and analyze multiple cardiac parameters such as left ventricular developed pressure, perfusion pressure, coronary flow, cardiac electrical activity (ECG/EKG), heart rate and temperature all in real-time. Typically, Langendorff perfusion is used to study ischemia-reperfusion injury, vascular reactivity, electrical conduction, and pharmacological interventions.
See here for more information about our Langendorff solutions.
Related: Effects of constant flow vs. constant pressure perfusion on Langendorff isolated heart studies.
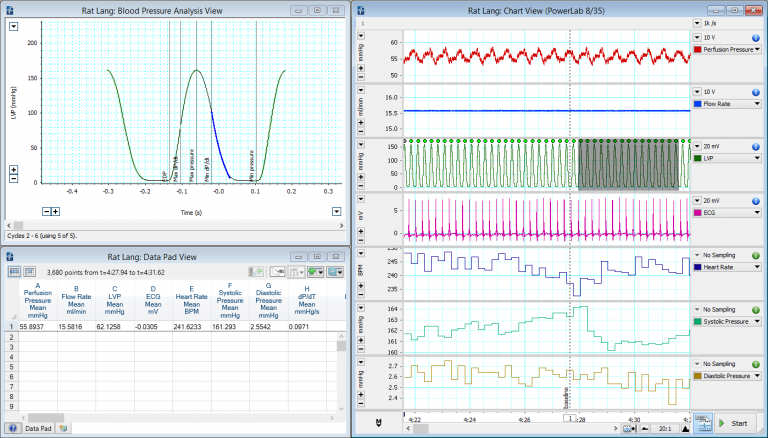
A typical Langendorff recording in LabChart (rat model) featuring LVP, ECG, perfusion pressure and calculated variables.
Typical isolated heart studies:
- Cardiac metabolism
- Medical device testing
- Artificial heart development
- Ischemia - reperfusion studies
- Pharmacology / toxicology studies
- Systolic and diastolic dysfunction
- Pulmonary hypertension
- Myocardial function
- Hypertrophy, infarction, cardiomyopathy, and other disease models
- Systemic circulation or ventricular studies
Hopefully, this has helped to clarify the differences between Working Heart and Langendorff perfusion models so you can decide which is the best solution for you!
Find out more:
An introduction to isolated Langendorff heart – Experimental considerations and best practices (Free on-demand webinar)
Priming and operating your Radnoti Working Heart system (video)
Three benefits of isolated organ research
12 pro tips for Langendorff technique
References
Liao R, Podesser BK, Lim CC 2012, The continuing evolution of the Langendorff and ejecting murine heart: new advances in cardiac phenotyping, Am J Physiol Heart Circ Physiol.
Bell RM, Mocanu MM, Yellon DM 2011, Retrograde heart perfusion: the Langendorff technique of isolated heart perfusion, J Mol Cell Cardiol.
